AI medical imaging workflow optimization is a practical way to make hospitals faster, smarter, and more accurate when they look inside patients. It turns the whole process—from taking the scan to giving a doctor a diagnosis—into a smooth, automated chain that learns from data. This article explains what it is, why it matters, how to build one, and how it can help you save time, reduce costs, and keep patients happier.
Why AI Medical Imaging Workflow Matters
Imagine a busy radiology department that takes a chest X‑ray, reads it, writes a report, and sends it back to the doctor. Even if each step is quick, small delays pile up. In a large hospital, this can mean a patient waiting hours for results. AI medical imaging workflow tackles this problem in a few clear ways:
- Faster Turnaround – AI can flag urgent findings while the scanner is still running, so doctors get alerts almost instantly.
- Better Accuracy – AI checks the report against thousands of previous cases, catching subtle patterns that a human might miss.
- Lower Cost – Automation cuts the number of people needed to process images, reducing labor costs.
- Consistent Quality – Every image is evaluated the same way, so variability between technicians or radiologists drops.
In short, AI medical imaging workflow is not just a fancy buzzword. It’s a set of tools that can move patients through the system more quickly and reliably.
The Building Blocks of an AI Medical Imaging Workflow
| Layer | What It Does | How AI Helps |
|---|---|---|
| Data Capture | Gets images from scanners (CT, MRI, X‑ray) and patient data from the hospital system | Formats everything into a standard that AI can read |
| Data Hub | Stores all images, reports, and metadata in one place | Enables fast search and easy access for AI |
| Pre‑Processing | Cleans images, corrects distortions, normalises contrast | Prepares data so AI sees consistent pictures |
| AI Models | Detects lesions, rates image quality, suggests diagnosis | Learns from thousands of past scans |
| Workflow Engine | Routes images to the right technician, radiologist, or AI | Keeps the pipeline moving without human bottlenecks |
| Reporting Tool | Builds readable reports, highlights key findings | Uses AI‑generated summaries that doctors can trust |
| Feedback Loop | Radiologists mark AI mistakes, data is re‑trained | AI gets better over time |
Sensors & Imaging Devices
Every hospital has a bunch of machines that capture pictures of the inside of the body. These could be X‑ray units, CT scanners, MRI machines, or ultrasound devices. The first job of the AI workflow is to get those images into the system in a standard format (usually DICOM). It also pulls in related data such as patient age, sex, and symptoms so the AI can consider the right context.
Data Hub and Cloud
A centralized storage that can hold millions of images and their associated data is essential. Many hospitals use a secure cloud or a private server that can store and serve images fast. The hub also handles backups and access control, so only the right people can see sensitive data.
Pre‑Processing
Raw images can have noise or different lighting levels. AI models perform a quick cleaning step that removes artifacts and normalises contrast. This makes the next stage—detection—more accurate.
AI Models for Detection and Diagnosis
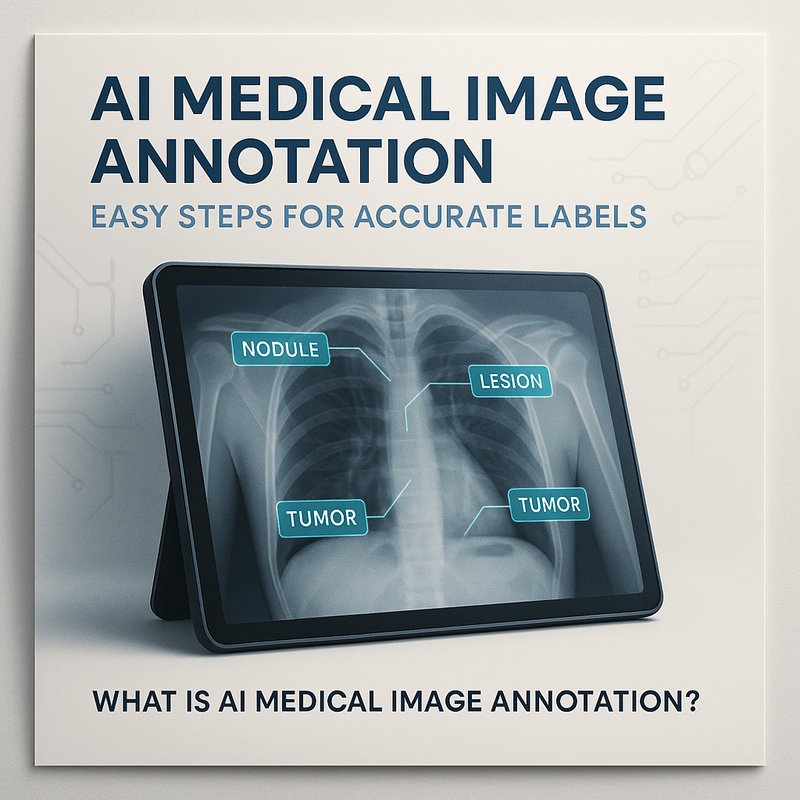
The core of the workflow is the AI model. Depending on the type of scan, the model may:
- Spot Tumors – Detect lung nodules on CT or breast lesions on mammography.
- Grade Image Quality – Tell if a scan is blurry or missing a slice.
- Suggest a Diagnosis – Based on pattern recognition, give a list of possible conditions ranked by probability.
These models are trained on large, labeled datasets that come from hospitals or public repositories. They are constantly re‑trained with new data to stay sharp.
Workflow Engine
Once the AI has finished its job, the workflow engine decides what to do next. For example:
- If the AI flags an urgent finding, the image is sent straight to a senior radiologist.
- If the image quality is low, the engine requests a repeat scan.
- If the AI is confident, it auto‑fills the report, allowing the radiologist to review quickly.
The engine is usually built on a rule‑based system that can be tuned by administrators. It can also learn over time which routes produce the fastest turnaround.
Reporting Tool
The final step is a readable report that includes the AI’s findings, image captions, and a short summary. Radiologists can quickly approve or adjust the report. The report is then sent back to the doctor’s electronic health record (EHR).
Feedback Loop
After a report is signed off, the radiologist can mark whether the AI was correct or not. That feedback is fed back into the training pipeline. In a few weeks, the AI model will have learned from the new data and improved its accuracy.
How to Build a Pilot AI Medical Imaging Workflow
A pilot is a small, controlled experiment that shows the benefits before you roll out the whole system. Here’s a step‑by‑step guide.
1. Set a Clear Goal
Pick one department or scan type to focus on. For example, “Reduce CT chest report turnaround from 4 hours to 1 hour in the emergency department.”
2. Inventory Your Resources
List all imaging machines, the IT systems they connect to, and the existing staff workflow. Identify gaps such as missing scanners or incomplete data.
3. Choose a Data Hub
If your hospital already has a cloud or on‑prem solution, you can use that. Otherwise, set up a secure storage that follows health data regulations (HIPAA, GDPR). Use a solution that can serve images quickly to AI.
4. Select AI Models

Start with pre‑trained models that match your scan type. Many companies offer open‑source or commercial models for lung nodule detection, breast cancer screening, or brain tumor segmentation. Adapt them to your local data using transfer learning.
5. Build the Workflow Engine
Use a low‑code workflow platform or custom scripts that read the hub, trigger AI inference, and route the results. Make sure the engine can be changed without touching the AI code.
6. Integrate Reporting
Use a reporting template that can ingest AI outputs. Many EHR vendors provide APIs that let you push structured reports. Make sure the report format matches clinical guidelines.
7. Set Up Feedback
Create a simple interface where radiologists can flag false positives or negatives. Store those labels back in the hub for retraining.
8. Run a 30‑Day Pilot
Deploy the system in one shift or one scanner. Monitor the key metrics:
| Metric | Target |
|---|---|
| Report turnaround time | < 2 hrs |
| AI accuracy (AUROC) | > 0.90 |
| Radiologist satisfaction | ≥ 80% positive |
| Cost per scan | Reduce by 20% |
Collect data and refine the pipeline.
9. Scale Gradually
If the pilot succeeds, expand to other scanners, add more AI models (e.g., MRI brain), or roll out to another department.
Real-World Success Stories
| Hospital | Challenge | AI Solution | Outcome |
|---|---|---|---|
| St. Mary’s Hospital | Long wait for CT chest results | AI‑driven triage and quality check | Turnaround dropped from 4 hrs to 1 hr |
| Mercy Clinic | Missed small lung nodules | Deep‑learning lung nodule detector | Detection rate increased 15% |
| City Medical Center | High workload for radiologists | AI auto‑reporting with review workflow | Radiologists saved 3 hrs per day |
These stories show that AI medical imaging workflow can deliver real, measurable gains.
Common Pitfalls and How to Avoid Them
| Pitfall | Fix |
|---|---|
| Poor data quality | Perform routine audits, replace faulty scanners, retrain models on clean data |
| Over‑reliance on AI | Keep radiologists in the loop, require human sign‑off |
| Regulatory gaps | Follow HIPAA/GDPR, get IRB approval if using patient data |
| Complex integration | Start with a single scanner, use APIs, involve IT early |
| Skewed datasets | Balance training data by age, sex, disease prevalence |
Avoiding these pitfalls keeps the system reliable and compliant.
Emerging Trends in AI Medical Imaging Workflow
- Federated Learning – Hospitals train models locally and share only updates, keeping data in‑house.
- Explainable AI – Visual heat‑maps help radiologists see why the AI made a decision.
- Edge Deployment – Running AI on the scanner itself to get instant feedback.
- Multi‑Modal Fusion – Combining imaging with genomics or lab results for richer insights.
Staying on top of these trends ensures your workflow remains future‑ready.
Quick Start Checklist
- [ ] Define a single scan type and a clear turnaround goal.
- [ ] Map the existing imaging‑to‑report pipeline.
- [ ] Pick a secure data hub that meets regulatory standards.
- [ ] Choose or train a pre‑built AI model for your scan.
- [ ] Build a lightweight workflow engine that can route images.
- [ ] Create a reporting template that accepts AI outputs.
- [ ] Set up a simple feedback interface for radiologists.
- [ ] Run a 30‑day pilot and measure key metrics.
- [ ] Iterate, scale, and repeat.
Take Action Today
If you’re a radiology department lead or a hospital IT manager, start by reviewing your current workflow. Identify the biggest bottleneck—usually the time it takes to get a report back. Then ask: can an AI‑driven image quality checker or a triage system cut that time?
Visit the Neura AI product page at https://meetneura.ai/products to see how their AI tools can be plugged into your existing systems. Check out real case studies https://blog.meetneura.ai/#case-studies to see how other hospitals have succeeded. Then schedule a pilot and watch the numbers improve.
AI medical imaging workflow isn’t a distant future. It’s a set of proven, practical steps that can start delivering faster, better diagnoses today.